welcome to week 3
Welcome to week three. This week is comprised of variety of topics. We’ll be talking about outpatient hypertension management to start the week. Blood pressure control is one of our best tools to combat morbidity and mortality in our patients and as such, it’s important to get it right. Secondly, we’ll be delving into central line placements. We have a Blue Phantom CVL simulator that we’re looking forward to using to help you improve your procedure skills. Lastly, we’ll be taking a stab at acid-base evaluation. We know that almost every time you are taught acid-base, it’s likely taught in an entirely new way and is always terribly confusing. It was to us too. This is not a new problem — and it won’t get better. There are so many ways to interpret acid-base (look no further than the Great Transatlantic Acid-Base Debate of the 1960s) that you just need to find a way that works for you for exams and real life and then commit it to memory. We’ll talk about an acid-base approach that works well for routine clinical practice and board exams.
Table of Contents
Management of Outpatient Hypertension
Ultrasound and CVL Simulation
Acid-Base Evaluation
Management of Outpatient Hypertension
Hypertension is often called the silent killer. It is estimated that approximately 45% of adults in the United States have uncontrolled blood pressure. In the southern states and along the delta, the statistic is even higher - around 52%. In November of 2017, the American College of Cardiology and the American Heart Association released a new set of guidelines that falls more in line with the JNC 7 recommendations of tighter blood pressure control, rather than the more recent JNC 8 recommendations. Normal blood pressure is defined as <120/80 with these new guidelines. Hypertension is currently staged according to the following parameters:
Elevated Blood Pressure : systolic between 120-129 mm Hg
Stage I: systolic between 130-139 OR diastolic between 80-89 mm Hg
Stage II: systolic at least 140 OR diastolic at least 90 mm Hg
Hypertensive urgency/emergency: *see section on inpatient hypertension management
The pathogenesis of hypertension continues to be perplexing and to date there is still no unifying mechanism. Potential underlying neural, hormonal, renal, and vascular mechanisms can all contribute to elevated blood pressure and thus treatment regimens can become complex and are not without side effects. Approximately 90% of patients with hypertension will have the diagnosis of Essential Hypertension, which means that the etiology is unknown. Risk factors for hypertension include both modifiable and non-modifiable attributes. When you are seeing a patient in any type of formal encounter, it is prudent to screen them for such risk factors and obtain a quality set of vital signs. This leads to our next part of outpatient management of blood pressure: a good quality blood pressure technique.
The gold standard for diagnosing hypertension continues to be ambulatory blood pressure monitoring (ABPM). ABPM allows for interpretation of the short-term variability of blood pressure over 24 hours and gives useful data in assessing for appropriate nighttime dipping. At NEA we have the Welch-Allyn device. It measures recordings every 30 minutes during the day and every hour during the night. A measurement of upper arm circumference is done and the brachial pulse is palpated and marked to ensure proper cuff size and placement. The current reimbursable diagnoses for ABPM includes essential hypertension, suspected white coat hypertension, and suspected masked hypertension.
Once a diagnosis of hypertension has been made, the next step is to prescribe the appropriate medication. The classic, first-line therapies should always be considered first. This includes calcium channel blockers, ACE/ARB, and thiazide or thiazide-like diuretics. For stage I hypertension, blood pressure control may be achieved with a single agent. For stage II hypertension, dual therapy should be initiated with moderate doses of medications. Most people will require at least two medications to achieve normotension. Maximizing a single agent has not been shown to improve blood pressure control, but rather often just increases adverse effects of medications. This is particularly true with diuretics.
How do you decide what medications to prescribe? The process starts with taking a very thorough history of the onset of hypertension, previous medications, and a review of lifestyle/habits. Compelling indications for certain classes of drugs can almost always be found if you pay attention to the patient history (example, diabetes = ACE/ARB, tachycardia = beta blocker). Calcium channel blockers, ACE/ARB, and thiazide or thiazide-like diuretics are considered first line therapies for hypertension. Calcium channel blockers and diuretics have been shown to be more effective at controlling blood pressure in African-Americans when used as monotherapy and have greater antihypertensive effects in the elderly due to pharmacokinetic changes as we age. Patients who are younger or who are nonblack, tend to respond better to renin-blocking drugs. Always remember that chlorthalidone and indapamide are stronger antihypertensives than HCTZ and are typically better tolerated when patients complain of leg cramps with thiazides (note: thiazides do not work well in patients with eGFR <30). When conventional antihypertensives at moderate to high doses -- and at least a moderate effort for lifestyle modification -- fail to control blood pressure, an MRA such as spironolactone should be considered as a 4th agent. Use of spironolactone in patients with eGFR <30 is somewhat controversial due to the risk of hyperkalemia. Following that, the medication choices may include agents such as beta-blockers, alpha-blockers, long acting nitrates, and finally centrally acting alpha agonists and direct vasodilators. When you have exhausted all appropriate medications, you can consider minoxidil as a last ditch effort to control blood pressure, particularly in hypertension associated with renal insufficiency. Using minoxidil is tricky and can be very risky. Approximately 3% of patients who take minoxidil develop pericardial effusions.
You will often see very elderly patients with hypertension. Patients over the age of 80 are currently the fastest growing demographic. The HYVET trial looked at 3845 individuals over the age of 80 with sustained systolic BP of 160 mm Hg or higher, with mean seated pressure of 173/91. Half were assigned to placebo and the other half to treatment, with a goal to achieve systolic pressure of 150 mm Hg. The treatment group achieved significantly greater protection against stroke, heart failure, and all-cause mortality after only 1.8 years. Thus the trial was stopped early. This important trial proved that patients at any age, with reasonable life expectancy, deserve to be treated with antihypertensives if their systolic pressure is 160 mm Hg or higher.
Hypertension is a very broad topic and it is difficult to convey all of the wisdom one needs in a single writing. The most important aspect of treating hypertension is to do just that -- treat it. Patients will often tell you that their blood pressure is “good at home” and my rebuttal to that is “prove it to me.” Encourage your patients to check their blood pressure at home and send the readings to you. Teach them the proper way to take a blood pressure at home. Empower them with knowledge about their medications and WHY getting blood pressure under control is so important. Help them understand what is acceptable control vs needs improvement vs life threatening signs/symptoms. Facilitate compliance with medication by using combination therapies when you can. Finally, here are a few other key points/tips to remember:
Drugs that vasodilate can cause edema (looking at you calcium channel blockers). This swelling will not, I repeat WILL NOT, respond to diuretic therapy. The way to treat that type of swelling is to decrease the dose or stop the medication.
Erectile dysfunction is a common complaint with hypertension. Sometimes hypertension medications can contribute to ED, especially diuretics. However, it is not always the medication’s fault. ED can be a clue into the likelihood of cardiovascular disease and may be the result of a bigger problem. Ask your male patients about ED when they have hypertension.
Diuretics have the capacity to potentiate the effect of all other types of antihypertensives. However, diuretics can also lead to multiple unwanted problems including electrolyte imbalance, hyperuricemia, increased insulin resistance, and effects on fat distribution. This is especially true when diuretics are used at high doses.
Quiz Questions
A 37 year old male patient presents to your clinic for a routine wellness visit. He has no significant past medical history. He takes ibuprofen on a regular basis for headaches and back pain. His blood pressure in your office is 147/90, HR 78, RR 18. His basic metabolic panel is unremarkable. What is the most appropriate next step in regards to his elevated blood pressure?
What is the most common cause of secondary hypertension?
How do you differentiate between hypertensive urgency and hypertensive crisis?
What is the classic triad associated with renal artery stenosis?
You are asked to evaluate a 53 year old male patient with early onset and difficult to control hypertension (average daily readings of 163/97) despite treatment with maximum dose amlodipine, maximum dose benicar, and 25 mg of chlorthalidone. His chemistry panel is unremarkable with the exception of a potassium of 3.1 and serum CO2 of 34. Besides resistant hypertension, what should you include in your differential diagnosis and what is the most appropriate next step in the treatment plan?
Ultrasound and CVL Simulation
text herre
Acid-Base Evaluation
To Start, read this approach to acid-base evaluation. It is the method that has worked for us.
Next, practice your acid-base skills with these examples:
Case 1
Case 2
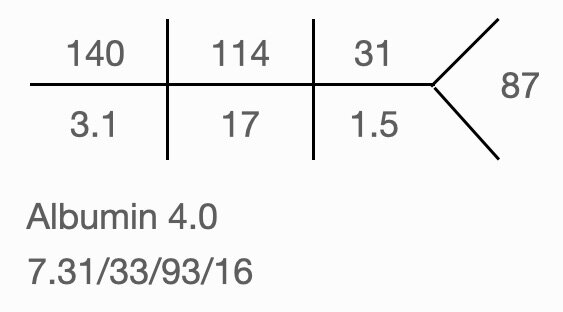
Called to Mr. Smith, a 83yo CM, who was found with altered mental status during routine vital signs check at midnight. Morphine IV 10mg was given 3h prior to exam.
Case 3
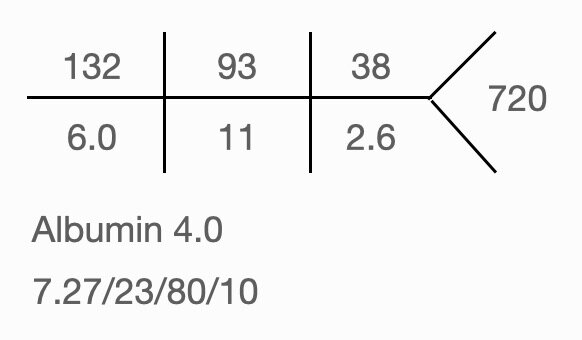
Called by ED physician to admit a 45yo CM with 3 days of severe watery diarrhea. Orthostatic vital signs positive and decreased skin turgor present.
Case 4
42yo man evaluated in the ED for AMS. Earlier today, he visited a homeopathic practitioner for psoriasis and was treated with cream and body wrap for 1h. He currently has nausea and reports hearing water in his ears.
Case 5
22 year old female with type I DM, presents to the emergency department with a 1 day history of nausea, vomiting, polyuria, polydipsia and vague abdominal pain. P.E. noted for deep sighing breathing, orthostatic hypotension, and dry mucous membranes. UA positive for ketones and glucose.
Case 6
41yo CM presenting to the ED with n/v, muscle cramps, muscle weakness and SOB. Physical exam significant for white paint ring around mouth.